In the medical realm, Dyspepsia icd 10 accurately treats patients, guaranteeing they receive the right interventions to relieve their discomfort. Dyspepsia, commonly known as indigestion, is a prevalent digestive disorder that affects millions worldwide. It encompasses a range of discomforting symptoms in the upper abdomen, including bloating, nausea, and a sensation of fullness after meals. While not a disease in itself, dyspepsia can significantly impact one’s quality of life.
Understanding its underlying causes is crucial for effective management. This blog aims to shed light on the Dyspepsia icd 10 coding for dyspepsia, offering a clear classification for medical professionals. Moreover, we’ll explore the potential triggers and delve into the diverse array of symptoms, providing valuable insights for those seeking relief from this common digestive ailment.
Dyspepsia, colloquially known as indigestion, is a prevalent gastrointestinal issue affecting individuals of all ages. In the medical realm, dyspepsia is classified under the Dyspepsia icd 10 code K30, facilitating precise documentation and diagnosis. This alphanumeric code serves as a universal language for healthcare professionals, streamlining communication and ensuring accurate billing for services related to dyspepsia.

Dyspepsia icd 10‘s categorization allows practitioners to differentiate dyspepsia from other digestive disorders, aiding in tailored treatment plans. It encompasses a spectrum of symptoms, including bloating, heartburn, and discomfort in the upper abdomen. Identifying the specific dyspepsia icd 10 code K30 for dyspepsia is the initial step toward effective management.
Although dyspepsia is not an illness in and of itself, it can be a sign of underlying conditions such as gastritis, acid reflux, or peptic ulcers. Healthcare professionals must be knowledgeable about Dyspepsia icd 10 coding to accurately treat patients, guaranteeing they receive the right interventions to relieve their discomfort and enhance their general quality of life.
What is Dyspepsia icd 10?
Dyspepsia icd 10, or International Classification of Diseases, 10th Edition, is a standardized coding system used by healthcare professionals globally to classify and document various medical conditions. Specifically, Dyspepsia icd 10 code K30 is assigned to dyspepsia, commonly known as indigestion. Dyspepsia icd 10 is a broad term encompassing a range of digestive discomforts, including bloating, nausea, abdominal pain, and a feeling of fullness after eating.
By employing the Dyspepsia icd 10 coding system, healthcare practitioners can accurately record and communicate diagnoses related to Dyspepsia icd 10. This coding not only aids in precise documentation but also assists in creating tailored treatment plans for patients. It allows for efficient tracking of patient data, facilitating research and healthcare management strategies.
Dyspepsia, while not a disease in itself, can be indicative of underlying gastrointestinal issues such as acid reflux, gastritis, or peptic ulcers. Understanding and utilizing the Dyspepsia icd 10 code K30 for dyspepsia is essential for healthcare providers, ensuring patients receive the appropriate care and interventions necessary for symptom relief and improved quality of life.
ALSO READ: Blood Sugar Chart and 20 Effective Ways For Boosting Wellness
Could you explain functional dyspepsia?
Functional dyspepsia is a chronic digestive disorder characterized by persistent pain or discomfort in the upper abdomen. Unlike other gastrointestinal conditions, functional dyspepsia doesn’t have an identifiable structural or biochemical cause. This makes it a functional disorder, meaning it arises from abnormal functioning rather than a specific underlying issue.
Bloating, early satiety (feeling full right away after eating), nausea, and occasionally heartburn are symptoms that people with functional dyspepsia frequently experience. Due to dietary limitations, decreased appetite, and emotional anguish, it may have a major influence on a person’s quality of life.
The exact cause of functional dyspepsia remains unclear, but factors such as abnormal gut motility, visceral hypersensitivity, and psychological factors may contribute. It is a common condition, affecting roughly 10-15% of the global population. While it can occur at any age, functional dyspepsia is more prevalent in adults, with a slightly higher incidence in females.
Effective management of functional dyspepsia often involves a combination of lifestyle modifications, dietary changes, and sometimes medication to alleviate symptoms and improve overall well-being. It’s essential for individuals experiencing these symptoms to seek medical advice for proper diagnosis and tailored treatment.
What is the prevalence of functional dyspepsia?
Functional dyspepsia is a relatively common gastrointestinal disorder, affecting a significant portion of the global population. Its prevalence is estimated to be around 10-15%, making it one of the most prevalent gastrointestinal conditions worldwide. This means that millions of individuals experience the chronic discomfort and symptoms associated with functional dyspepsia.
While functional dyspepsia can affect people of all ages, it is crucial to remember that it is typically diagnosed in adults. Additionally, the incidence rates may vary slightly according to variables including geographic location and demographic characteristics.
The condition’s high prevalence underscores the need for effective management and treatment strategies. Given its impact on daily life and overall well-being, individuals experiencing symptoms of functional dyspepsia should seek medical attention for proper diagnosis and guidance. Through understanding its prevalence and seeking appropriate care, those affected by functional dyspepsia can work towards improved quality of life and relief from their symptoms.
Causes Of Dyspepsia icd 10:
Gastroesophageal Reflux Disease (GERD)
Gastric or Peptic Ulcers
Helicobacter pylori Infection
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) Usage
Functional Dyspepsia (Unknown Underlying Cause)
Gastroparesis
Pancreatitis
Gallstones
Chronic Pancreatitis
Stomach Cancer (Rare, but a possible cause)
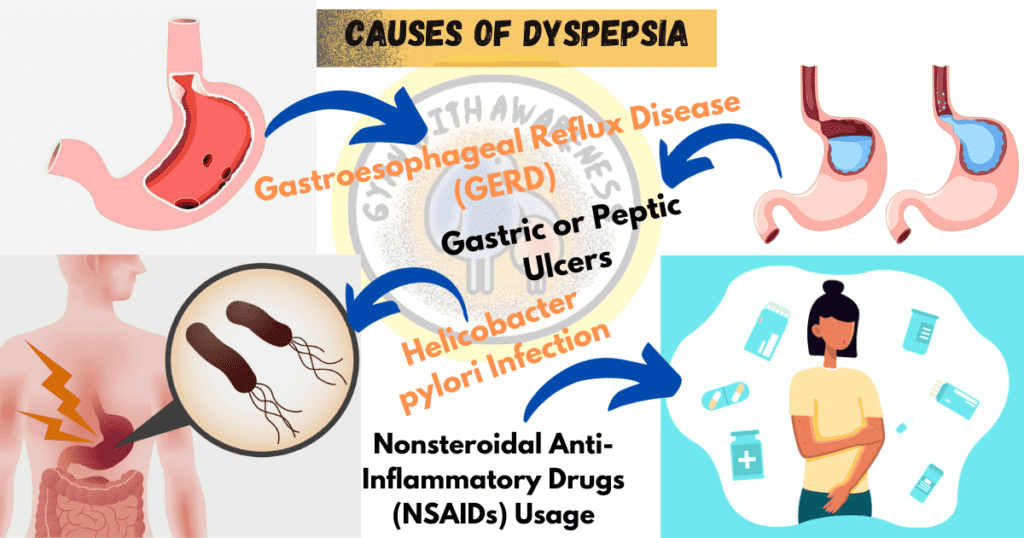
GERD, also known as gastroesophageal reflux disease, is a disorder where stomach acid backs up into the esophagus, causing symptoms like heartburn and discomfort in the upper abdomen.
Peptic Ulcers: Visible sores in the stomach or duodenum lining brought on by an imbalance in the digestive juices.
Infection with Helicobacter pylori: A bacterial infection that may result in stomach lining inflammation and maybe dyspeptic symptoms.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Aspirin and ibuprofen, two common NSAIDs, can irritate the stomach lining and cause dyspepsia when used for a prolonged period.
When there is no clear cause for the indigestion symptoms, they are referred to as functional dyspepsia.
Chronic Pancreatitis: Long-term inflammation of the pancreas can lead to persistent digestive problems, including dyspepsia.
Stomach Cancer: Though relatively rare, stomach cancer can present with dyspeptic symptoms, especially in advanced stages.
Gastroparesis is characterized by a delayed emptying of the stomach, which causes discomfort, pain, and bloating.
Pancreatic inflammation: Along with other digestive issues, pancreatic inflammation can present as dyspepsia symptoms.
Gallstones: Gallstones can produce several symptoms, including dyspepsia when they block the bile ducts.
Role of Dyspepsia icd 10 In pregnancy Time:
AccurateDyspepsia icd 10 coding helps in accurately identifying and documenting Dyspepsia icd 10 during pregnancy.
Tailored Treatment Plans: It enables healthcare providers to create specific treatment strategies for pregnant individuals experiencing Dyspepsia icd 10.
Monitoring and Follow-up: Dyspepsia icd 10 coding aids in tracking the progress of dyspepsia symptoms throughout the pregnancy.
Insurance and Billing: Proper coding ensures accurate billing and insurance claims, facilitating smoother financial processes for both patients and healthcare facilities.
Research and Data Analysis: Dyspepsia icd 10 allows for the collection of data on dyspepsia in pregnancy, aiding in research and the development of effective interventions.
Risk Assessment: It helps in evaluating any potential risks or complications associated with dyspepsia during pregnancy.
Documentation for Medical Records: Dyspepsia icd 10 codes provide essential information for maintaining comprehensive medical records, ensuring continuity of care.
Communication between Healthcare Providers: Standardized coding enhances communication among different healthcare professionals involved in the care of pregnant individuals with Dyspepsia icd 10.
Evidence-Based Practice: It supports evidence-based decision-making in the management of dyspepsia during pregnancy.
Quality Assurance: ICD-10 coding contributes to maintaining high standards of care by ensuring that appropriate diagnostic and treatment protocols are followed for pregnant individuals experiencing dyspepsia.
Symptoms Of icd 10 dyspepsia:
Upper Abdominal Pain or Discomfort: Persistent pain or discomfort in the upper abdomen is a hallmark symptom of dyspepsia.
Bloating: Many individuals with dyspepsia experience a sensation of fullness or bloating, even after consuming small meals.
Nausea: Dyspepsia can lead to feelings of queasiness or an urge to vomit, especially after eating.
Early Satiety: Individuals may feel full shortly after starting a meal, which can lead to decreased appetite.
Heartburn: Some may experience a burning sensation in the chest or throat, particularly after consuming spicy or acidic foods.
Belching or Excessive Gas: Dyspepsia can lead to increased belching or passing of gas.
Indigestion: A general feeling of discomfort or unease in the upper abdomen is a common symptom.
Regurgitation: Some individuals may experience the return of food or stomach acid into the mouth.
Unexplained Weight Loss: In some cases, chronic dyspepsia can lead to unintended weight loss.
Fatigue: Chronic discomfort and disrupted digestion can lead to a general sense of fatigue and decreased energy levels.
It’s important to note that while these are common symptoms of dyspepsia, individual experiences may vary. Seeking professional medical advice for accurate diagnosis and appropriate treatment is crucial for those experiencing these symptoms.

Signs That Indicate You Should Consult a Doctor:
Unintentional Weight Loss: If you find yourself losing weight without intending to, this may indicate a serious health problem that needs to be addressed.
Swallowing Difficulties: It’s important to consult a doctor if you have trouble swallowing, especially if it comes with pain or discomfort.
Vomiting Blood or Dark Material: This may be a sign of internal bleeding, which is a significant worry and calls for prompt medical care.
Stools that are black or tarry may indicate gastrointestinal bleeding and require investigation by a physician.
Constant or Extreme discomfort: If you are having constant or extreme stomach discomfort, especially if it is getting worse, get emergency medical assistance.
Frequent or Severe Heartburn: Chronic or severe heartburn, especially if it’s not relieved by over-the-counter medications, should be discussed with a healthcare provider.
Persistent Nausea or Vomiting: If you’re frequently nauseated or vomiting for an extended period, medical assessment is crucial.
Difficulty Breathing: If dyspeptic symptoms are accompanied by difficulty breathing or chest pain, seek medical help immediately.
Family History of Digestive Disorders: If there’s a family history of conditions like stomach cancer, ulcers, or other gastrointestinal issues, it’s advisable to consult a doctor.
New Onset of Symptoms in Middle-Aged or Older Adults: Any sudden onset of dyspeptic symptoms in middle-aged or older individuals should be evaluated by a healthcare professional.

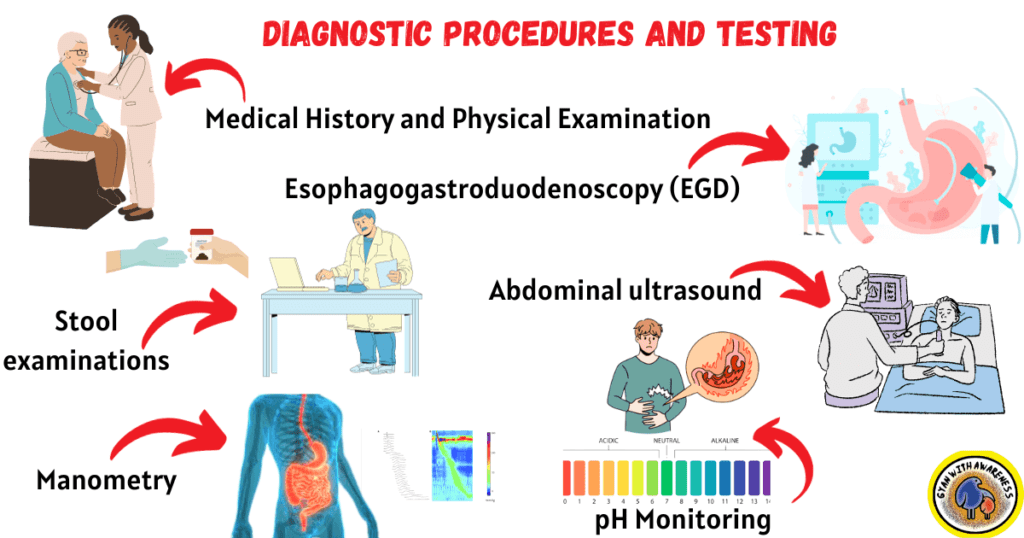
Diagnostic Procedures and Testing:
Medical History and Physical Examination: The initial stage comprises discussing symptoms, compiling a medical history, and carrying out a thorough physical examination to ascertain potential causes.
To check for signs of an infection, anemia, or other irregularities, blood tests may be carried out.
Stool examinations: These examinations can assist in identifying the presence of blood or diseases in the gastrointestinal system.
Esophagogastroduodenoscopy (EGD): This procedure uses a flexible tube equipped with a camera to look for abnormalities in the lining of the esophagus, stomach, and duodenum.
After consuming a barium solution, a series of X-rays are performed to highlight the upper digestive tract.
Abdominal ultrasound: This imaging method can be used to find problems with the pancreas, liver, or gallbladder.
A detailed image of the abdomen is provided by a CT scan or an MRI, which aids in the identification of any structural anomalies.
pH Monitoring: Determines the degree of acidity in the esophagus to check for acid reflux, which may be the root of dyspepsia.
The gastric emptying study measures how rapidly food passes through the stomach and can be used to identify diseases like gastroparesis.
Manometry: Checks for motility abnormalities by measuring the pressure and contractions in the esophagus.
Approaches for Managing and Treating Dyspepsia:
Lifestyle Modifications:
- Adopting a balanced diet rich in fiber, fruits, and vegetables.
- Avoiding trigger foods like spicy, greasy, or acidic items.
- Eating smaller, more frequent meals throughout the day.
Avoiding Irritants:
- Minimizing alcohol consumption and tobacco use.
- Limiting intake of caffeine-containing beverages.
Stress Reduction:
- Practicing relaxation exercises like yoga, meditation, or deep breathing.
- Regular exercise can assist digestion and reduce stress.
Medications available over-the-counter (OTC):
- Antacids help reduce heartburn and neutralize stomach acid.
- To lessen the production of stomach acid, use H2-receptor antagonists or proton pump inhibitors (PPIs).
Medications on prescription:
- Prokinetics help speed up digestion and increase stomach emptying.
- Treatments for underlying illnesses such as Helicobacter pylori infection.
Nutritional advice:
Collaborating with a dietician to create a personalized meal plan that satisfies the needs of the person.
Psychological assistance
For those suffering from stress- or anxiety-related dyspepsia, therapy or counseling may be helpful.
Treatments to empty the stomach:
Treatment options for gastroparesis may include drugs that increase stomach motility, surgery, or, in more serious cases, gastric electrical stimulation.
Surgery:
For some underlying causes of dyspepsia, such as peptic ulcers or severe reflux, surgery may in rare instances be advised.
Regular Follow-up:
Routine check-ups with a healthcare provider to monitor progress and adjust treatment as needed.
Alternative Therapies:
Some individuals find relief through practices like acupuncture, herbal remedies, or probiotics. It’s important to discuss these options with a healthcare provider.
Clinical Trials and Research:
Participating in clinical trials for innovative treatments or therapies under the guidance of healthcare professionals.
Nutritional Strategies for Managing Dyspepsia icd 10:
To reduce the stress on the digestive system, smaller, more frequent meals are advised throughout the day.
Avoid Trigger Foods: Be aware of foods that can aggravate dyspeptic symptoms, such as spicy, acidic, or high-fat foods, and stay away from them.
Limit Coffee and Caffeine: Limit your intake of coffee and other caffeinated beverages because they may worsen symptoms by promoting the formation of stomach acid.
Reducing alcohol consumption is a good idea because it can irritate the digestive tract.
Pick Low-Fat Options: Choose lean meats, low-fat dairy products, and cooking techniques that use little to no oil or grease.
Incorporate fruits, vegetables, whole grains, and foods high in fiber to help with good digestion and regular bowel movements.
Keep Hydrated: To promote overall digestive health, drink lots of water throughout the day.
Take your time and chew your food completely to promote mindful eating and better digestion.
Consider Probiotics: Probiotic-rich foods or supplements may help promote a healthy balance of gut bacteria.
Avoid Late-Night Eating: Refrain from consuming large meals or snacks close to bedtime to allow for proper digestion before lying down.
Keep a Food Diary: Tracking what you eat and any associated symptoms can help identify specific triggers and tailor your diet accordingly.
A healthy balance of gut flora may be promoted by probiotic-rich foods or supplements, so consider these.
Avoid Late-Night Eating: To allow for proper digestion before lying down, avoid ingesting heavy meals or snacks close to bedtime.
Also Read: The Benefits of Tofu: Best Diabetes-Friendly Food, Part 12
Diabetes Cure | Best Mediterranean Chickpea Salad | Part 11
Innovative Grilled Salmon Recipes | Diabetes Cure | Part 10
Diabetes Cure | Delicious Barley Vegetable Soup | Part 9
Delicious Gooseberry Chutney | Diabetes Cure | Part 8
Exquisite Lentil Salad | Diabetes Cure Recipes | Part 7
Best Diabetes Cure | Grilled Fish Recipes | Part 6
Best Diabetes Cure | Brazil Nuts Recipes | Part 5
Best Diabetes Cure | Greek Yogurt Smoothie Recipes | Part 4
Best Diabetes Cure | Greek Salad Recipe | Part 3
Powerful Diabetes Cure Recipes | Detox Island Green Smoothie | Part 2
Best Diabetes Cure | Curd Rice Recipe | Part 1
FAQ:
What is the diagnosis of Dyspepsia icd 10?
The diagnosis of Dyspepsia according to Dyspepsia icd 10 is coded as K30. This alphanumeric code serves as a standardized classification system used by healthcare professionals for accurate documentation and billing related to dyspepsia. It allows for precise identification of the condition, aiding in the development of tailored treatment plans for individuals experiencing symptoms of Dyspepsia icd 10.


1 thought on “Dyspepsia icd 10 Code, Causes, Symptoms, and Best Treatment”