Indigestion, a common ailment experienced by people of all ages, can cast a shadow on even the brightest of days. Its discomforting symptoms, ranging from bloating and abdominal pain to heartburn and nausea, can disrupt daily routines. Understanding the root causes of indigestion is the cornerstone of finding relief. In this comprehensive guide, we delve into the intricacies of indigestion, exploring its symptoms, uncovering its underlying triggers, and offering ten effective treatments. Whether you’re seeking immediate relief or long-term management, this resource aims to empower you with knowledge and actionable strategies to reclaim comfort and well-being. Join us on this journey to decode indigestion and pave the way towards a more comfortable, digestive-friendly life.
Indigestion, often regarded as a minor inconvenience, has a knack for making its presence known at the most inconvenient times. Those discomforting bouts of bloating, stomach pain, and heartburn can throw a wrench into even the best-laid plans. In this comprehensive guide, we’ll embark on a journey to unravel the mysteries of indigestion, exploring its diverse symptoms and the underlying culprits that lead to these unwelcome sensations.
Armed with this knowledge, we’ll then dive into a curated list of ten effective treatments, providing you with practical strategies to reclaim control over your digestive comfort. Whether you’re seeking quick relief or long-term solutions, this resource aims to equip you with the insights and tools needed for a more comfortable, indigestion-free life. So, let’s navigate through the realm of indigestion together and pave the way toward digestive well-being.
Also Read: The Benefits of Tofu: Best Diabetes-Friendly Food, Part 12
Diabetes Cure | Best Mediterranean Chickpea Salad | Part 11
Innovative Grilled Salmon Recipes | Diabetes Cure | Part 10
Diabetes Cure | Delicious Barley Vegetable Soup | Part 9
Delicious Gooseberry Chutney | Diabetes Cure | Part 8
Exquisite Lentil Salad | Diabetes Cure Recipes | Part 7
Best Diabetes Cure | Grilled Fish Recipes | Part 6
Best Diabetes Cure | Brazil Nuts Recipes | Part 5
Best Diabetes Cure | Greek Yogurt Smoothie Recipes | Part 4
Best Diabetes Cure | Greek Salad Recipe | Part 3
Powerful Diabetes Cure Recipes | Detox Island Green Smoothie | Part 2
Best Diabetes Cure | Curd Rice Recipe | Part 1
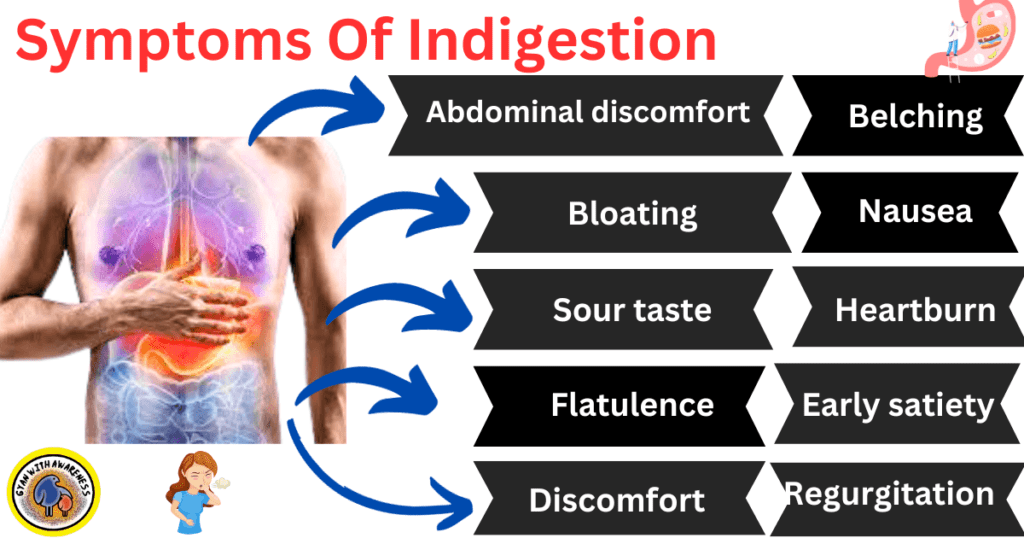
Symptoms Of Indigestion:
General discomfort or pain in the upper abdomen is referred to as abdominal discomfort.
Bloating: An abdominal feeling of fullness or swelling that frequently includes gas.
A burning sensation that may extend up into the throat is referred to as heartburn.
The feeling of being nauseated or they want to vomit.
Early satiety is the rapid onset of fullness following the commencement of a meal, even with small servings.
Belching excessively is when the stomach frequently releases air through the mouth.
A sour or bitter sensation in the mouth that is frequently related to acid reflux.
Regurgitation: The act of vomiting stomach acid or partially digested food back into the mouth.
A feeling of excessive acidity or sourness in the stomach is referred to as an acidic or sour stomach.
Difficulty in Swallowing: Sensation of food getting stuck or difficulty in passing it down the esophagus.
Common Causes of Indigestion:
Dietary Options: Eating meals that are hot, greasy, or excessively fatty can cause indigestion.
Overeating: Eating a lot at once or in excessive portions can tax the digestive system.
Gastroesophageal Reflux Disease: Indigestion symptoms can be brought on by acid reflux from the stomach into the esophagus.
Helicobacter pylori Infection: This bacterium can infect the stomach lining and contribute to indigestion.
Medications: Some drugs, especially nonsteroidal anti-inflammatory drugs, can irritate the stomach lining.
Anxiety and Stress: For some people, emotional stress can worsen indigestion symptoms.
Smoking: The lower esophageal sphincter may relax as a result of tobacco use, allowing stomach acid to reflux back into the esophagus.
Alcohol: By irritating the stomach lining, excessive alcohol use can cause indigestion.
Gallstones, peptic ulcers, and gastritis are a few examples of digestive conditions that could be present in the background.
Delayed Gastric Emptying: The condition of gastroparesis, which causes the stomach to take longer to empty its contents, can cause indigestion.
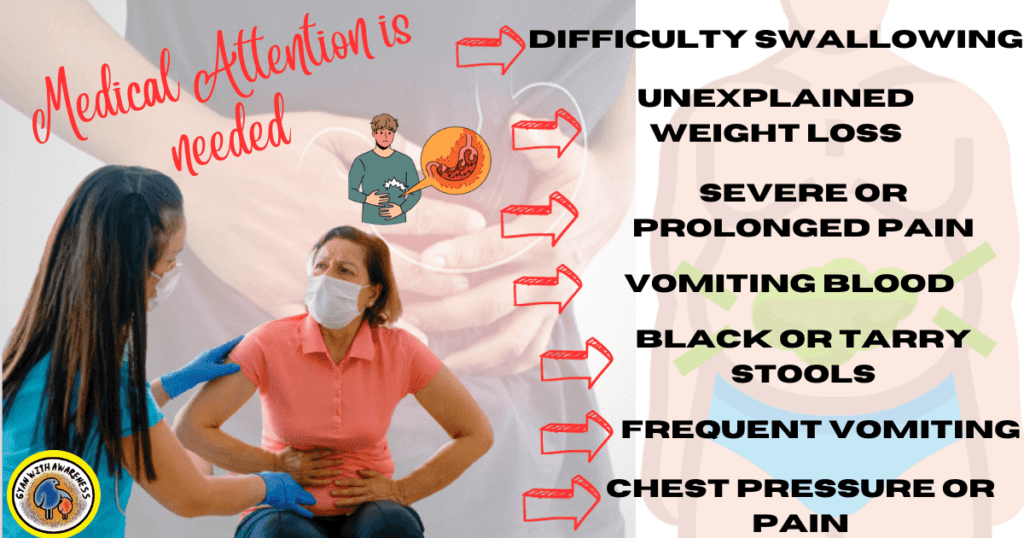
Signs Indicating a Need for Medical Attention:
Severe or Prolonged Pain: Intense or long-lasting abdominal pain, especially if it’s getting worse.
Difficulty Swallowing: Persistent difficulty in swallowing, or a feeling of food getting stuck in the throat.
Unexplained Weight Loss: Significant weight loss without intentional changes in diet or exercise.
Vomiting Blood: Presence of blood in vomit or material that resembles coffee grounds.
Black or Tarry Stools: This may indicate bleeding in the digestive tract.
Frequent Vomiting: Persistent vomiting, especially if it’s accompanied by other concerning symptoms.
Chest pressure or pain: This can be an indication of a heart condition, especially if it radiates to the arm, neck, or jaw.
Breathing problems, particularly if they are sudden or severe, include shortness of breath.
If you have a family history of digestive disorders such as stomach cancer, ulcers, or other gastrointestinal problems.
New Onset of Issues in Middle-Aged or Older Adults: A healthcare provider should be seen for any abrupt onset of digestive issues in this age range.
Potential Complications:
Esophageal Stricture: Chronic indigestion-related acid reflux can cause the esophagus to constrict, making swallowing challenging.
Barrett’s Esophagus: Prolonged, severe acid reflux can alter the structure of the esophageal lining, increasing the risk of esophageal cancer.
Peptic Ulcers: Stomach or duodenal ulcers can develop if untreated indigestion is brought on by Helicobacter pylori infection or overproduction of acid.
Gastric bleeding can result from persistent stomach lining irritation and inflammation.
Malnutrition: Severe or chronic indigestion can impair the body’s ability to absorb nutrients, leading to malnutrition.
Gastric Outlet Obstruction: In severe cases, chronic inflammation can cause a blockage in the stomach’s outlet, leading to difficulty in food passage.
Respiratory Problems: In cases of severe acid reflux, stomach acid can enter the respiratory tract, causing coughing, wheezing, or aspiration pneumonia.
Gastroesophageal Strictures: Repeated acid exposure can lead to the narrowing of the lower esophagus.
Psychological Impact: Chronic indigestion can lead to anxiety, depression, or other mental health issues.
Reduced Quality of Life: Persistent discomfort and pain can significantly impact daily activities, work, and overall well-being.
Acid Indigestion:
A common digestive ailment defined by the regurgitation of stomach acid into the esophagus is recognized clinically as gastroesophageal reflux disease (GERD), sometimes known as acid indigestion. The lower esophageal sphincter, a muscle ring that divides the stomach from the esophagus, has become less effective, causing acid to back up into the esophagus. The ensuing symptoms, which are sometimes referred to as heartburn, can be unpleasant and include a burning sensation in the chest.
Along with a sour or acidic taste in the mouth, swallowing issues, and sporadic coughing or hoarseness, those with acid indigestion may also suffer these symptoms. Usually, these feelings get worse after meals, especially when sitting or bending over.
Chronic acid indigestion can lead to more serious complications such as esophageal strictures, Barrett’s esophagus, and even an increased risk of esophageal cancer. Lifestyle modifications, including dietary changes, weight management, and avoiding triggering foods, play a crucial role in managing acid indigestion. Additionally, medications like proton pump inhibitors (PPIs) and H2-receptor antagonists can help reduce stomach acid production, providing relief for individuals affected by this condition. In severe cases, surgical interventions may be considered. Seeking timely medical attention and adhering to recommended treatment plans are essential for effectively managing acid indigestion and preventing complications.
Indigestion vs. heartburn:
Indigestion and heartburn are related yet distinct digestive discomforts. Indigestion, also known as dyspepsia, is a broad term encompassing a range of symptoms related to the digestive system. Heartburn vs. indigestion may include bloating, abdominal pain, nausea, and a feeling of fullness after eating. This condition can be caused by various factors, such as dietary choices, stress, or underlying digestive disorders.
On the other hand, gastroesophageal reflux disease has heartburn as a distinct symptom. Burning in the chest and an often acidic mouth taste are among the symptoms. When the lower esophageal sphincter weakens, stomach acid can reflux into the esophagus and cause this condition.
Heartburn is largely distinguished by a characteristic burning feeling, whereas indigestion includes a wider range of digestive discomforts. Heartburn vs. indigestion is crucial to distinguish between the two because they could have different underlying causes and call for different management and treatment strategies. For a precise diagnosis and customized therapies, speaking with a healthcare expert is essential.
DIY Solutions for (Home Remedies):
Ginger Tea: Ginger is known for its digestive properties. Drinking ginger tea can help alleviate indigestion.
Peppermint Oil: Peppermint oil capsules can help relax the muscles of the GI tract, reducing symptoms of indigestion.
Tea made from chamomile: Chamomile tea has anti-inflammatory and digestive-system soothing effects. Taking chamomile tea could be therapeutic.
Baking Soda: Baking soda can neutralize stomach acid when mixed with water to form an antacid.
Lemon Water: Digestion can be aided by consuming warm water with lemon juice to increase the formation of digestive juices.
Foods High in Probiotics: Probiotic foods like yogurt, kefir, and kefir can help maintain a healthy gut microbiome and enhance digestion.
Apple cider vinegar: Despite being naturally acidic, apple cider vinegar can aid in balancing the pH levels in the stomach, potentially reducing indigestion.
Fennel Seeds: Chewing on these seeds after a meal may aid in digestion and ease symptoms like bloating.
Aloe Vera Juice: Aloe vera juice helps ease stomach symptoms and soothe the digestive system.
Fresh mint leaves can be chewed and have a relaxing effect on the stomach, which can help with indigestion.
Indigestion During Pregnancy:
Common Occurrence: Indigestion, also known as dyspepsia, is a frequent discomfort experienced by pregnant individuals.
Hormonal Changes: Fluctuating hormone levels, particularly an increase in progesterone, can relax the digestive tract muscles, leading to slower digestion and potential indigestion.
Symptoms: Pregnant individuals with indigestion may experience symptoms such as heartburn, bloating, nausea, and a feeling of fullness after eating.
As the pregnancy goes on, the expanding uterus puts pressure on the stomach, possibly leading to acid reflux into the esophagus.
Elevating the Upper Body: Using extra pillows to elevate the upper body during sleep can reduce nighttime heartburn.
Avoiding Late-Night Snacking: Refraining from consuming large meals or snacks close to bedtime allows for proper digestion before lying down.
Dietary Modifications: A balanced diet rich in fiber, fruits, and vegetables will help manage indigestion. Trigger foods like spicy or oily foods should be avoided.
Smaller, More Regular Meals: Eating smaller, more regular meals can help reduce the stress on the digestive system.
Consulting a Healthcare Provider: If indigestion symptoms persist or worsen, seeking medical advice is crucial to rule out any underlying complications.
Treatment Options: In more severe cases, a healthcare provider may recommend over-the-counter antacids or other medications safe for pregnancy to alleviate symptoms.
How long does Indigestion Last?
The duration of indigestion can vary widely depending on the underlying causes and individual factors. In many cases, indigestion is temporary and may last for a few hours to a day. It can be triggered by specific dietary choices, overeating, or consuming certain foods that are harder to digest.
However, for some individuals, especially those with chronic conditions like gastroesophageal reflux disease (GERD), indigestion can be a recurring issue that lasts for weeks, months, or even longer. In these cases, seeking medical advice is crucial to identify and address the underlying causes.
In addition, making lifestyle and nutritional adjustments as well as receiving the right medical care can greatly reduce the frequency and length of indigestion episodes. For thorough assessment and advice, speak with a healthcare professional, especially if your indigestion becomes chronic or recurrent.
Chest Pain Due to it:
Chest pain attributed to indigestion, often referred to as non-cardiac chest pain, is a discomforting sensation in the chest that arises from digestive issues rather than heart-related problems. This type of chest pain is typically characterized by a burning or sharp sensation and is commonly experienced in the upper abdomen or just below the breastbone. It may be accompanied by other symptoms of indigestion such as bloating, belching, and a feeling of fullness.
The condition known as gastroesophageal reflux disease, which causes the stomach acid to reflux into the esophagus, is typically what causes the pain. This reflux may cause chest pain by irritating the delicate esophageal lining. While chest pain caused by indigestion is not specifically linked to heart problems, it can mirror the symptoms of a heart attack and raise suspicion.
To rule out any significant cardiac conditions, it is imperative to get prompt medical assistance if chest discomfort is experienced, especially if it is the first time it has occurred or if it is severe or chronic. To ascertain the origin of the chest pain and suggest the most suitable course of action, a healthcare professional can conduct a full evaluation.
FAQ:
Indigestion presents with what signs?
Upper Abdominal Pain: Upper abdominal pain or discomfort that is persistent or recurrent.
Bloating: A feeling of fullness that is frequently accompanied by an enlarged abdomen.
Heartburn: A burning or uncomfortable feeling in the chest region, often after eating or after lying down.
Excessive Belching: Frequent burping, often in an attempt to relieve discomfort.
Acidic Taste or Sour Burps: A taste of stomach acid in the mouth or occasional sour burps.
What measures can be taken to alleviate indigestion?
Effective management of gas and anxiety requires a multifaceted strategy that takes into account both physical and psychological factors. First of all, making dietary changes can greatly minimize gas production. This includes staying away from items that cause gas, such as beans, certain vegetables, and carbonated beverages. Additionally, regular exercise helps facilitate healthy digestion and lessen gas buildup.
Stress-relieving strategies must be used to combat anxiety. Meditation, mindfulness training, and deep breathing techniques can all assist in calming the mind and reducing worry. Regular physical activity also releases endorphins, which have a calming, mood-stabilizing effect. Getting help from a mental health professional or participating in support groups can offer coping mechanisms and a secure setting to talk about anxiety-related issues.
Can stress contribute to the onset of indigestion?
Yes, stress can significantly contribute to the onset of indigestion. When a person is stressed, the body’s natural “fight or flight” response is triggered, which can affect the digestive system. This physiological response leads to the release of stress hormones like cortisol and adrenaline, which in turn can disrupt normal digestive processes.
Stress can lead to a variety of gastrointestinal issues, including increased stomach acid production, delayed gastric emptying, and changes in gut motility. These alterations can result in symptoms like heartburn, bloating, and abdominal discomfort – all hallmark signs of indigestion. Furthermore, stress may exacerbate pre-existing digestive conditions such as gastroesophageal reflux disease (GERD) or irritable bowel syndrome (IBS).
How can both gas and anxiety be managed effectively?
Effective management of gas and anxiety requires a multifaceted strategy that takes into account both physical and psychological factors. First of all, making dietary changes can greatly minimize gas production. This includes staying away from items that cause gas, such as beans, certain vegetables, and carbonated beverages. Additionally, regular exercise helps facilitate healthy digestion and lessen gas buildup.




3 thoughts on “Decoding Indigestion: Symptoms, Causes, and 10 Effective Treatments”