Leprosy, also known as Hansen’s disease, stands as one of the oldest and most stigmatized afflictions in human history. This chronic bacterial infection, caused by the bacterium Mycobacterium leprae, primarily targets the skin and nerves, leading to a range of distressing symptoms. Its historical associations with social ostracization have further shrouded leprosy in myth and misunderstanding.
The causative agent, Mycobacterium leprae, is a slow-growing bacterium that primarily targets the peripheral nerves and skin cells. This intricate interaction between the bacterium and the human immune system results in the distinct symptoms and clinical presentations associated with leprosy.

Symptomatically, leprosy manifests in various forms, ranging from mild skin lesions to severe nerve damage. Early signs often include pale or reddish skin patches with diminished sensation. As the disease advances, nerve involvement can lead to muscle weakness, loss of sensation, and deformities, particularly in the extremities.
The understanding and treatment of leprosy have advanced recently. To halt the spread of the disease and stop further advancement, a combination of multi-drug therapy has proven to be quite successful. In addition, rehabilitation and surgical procedures are essential for reducing the limitations that come with advanced instances. Hope is offered to those who are impacted by leprosy by this all-encompassing strategy that addresses medical, social, and rehabilitation issues. It aims to reduce physical suffering as well as the deeply embedded social shame that has historically surrounded this old disease.
Define leprosy:
A chronic infectious disease called leprosy, commonly referred to as Hansen’s disease, is brought on by the bacteria Mycobacterium leprae. The skin and nerves are the primary targets of this slow-growing bacterium, which can cause a variety of clinical symptoms. Leprosy is spread through infected people’s respiratory droplets, albeit it is not particularly contagious, and prolonged close contact is typically necessary for transmission.
The disease presents in various forms, with two main classifications: paucibacillary and multibacillary, based on the number of bacteria present in the body. Early symptoms often include skin lesions or patches that may be discolored and have diminished sensation. As leprosy progresses, it can lead to nerve damage, resulting in muscle weakness, loss of sensation, and deformities, particularly in the extremities.
Historically, leprosy carried a significant social stigma, leading to the isolation and discrimination of affected individuals. However, with advances in medical understanding and the availability of multi-drug therapy, the prognosis for leprosy has greatly improved. Early diagnosis and prompt treatment are crucial in preventing complications and disability associated with the disease. Efforts in education, awareness, and destigmatization continue to be important components in the global fight against leprosy.
Also Read: Eyesight! Expert Tips for Enhancing and 8 Healthy Food
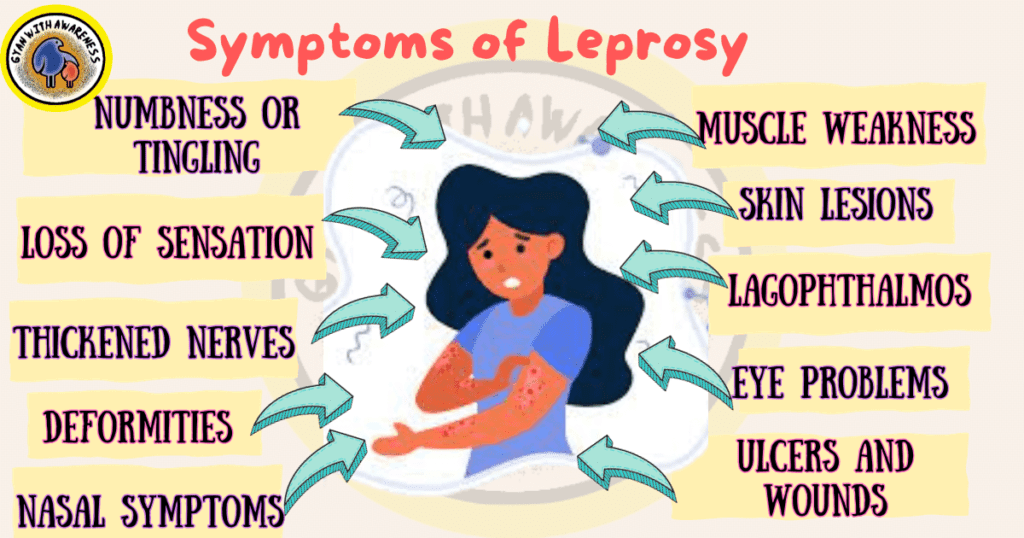
Symptoms of Leprosy
Skin Lesions: Leprosy often presents as discolored skin patches that may be lighter or reddish.
Loss of Sensation: Affected areas may have reduced or no sensation to touch, heat, or pain.
Numbness or Tingling: Patients may experience sensations of tingling or numbness in the skin.
Muscle Weakness: Nerve damage can lead to muscle weakness, particularly in the extremities.
Thickened Nerves: Nerves may become enlarged and palpable under the skin.
Eye Problems: In some cases, leprosy can affect the eyes, leading to issues like dryness, irritation, and decreased blinking reflex.
Nasal Symptoms: Leprosy can lead to nasal congestion and, in severe cases, nasal collapse.
Ulcers and Wounds: Advanced cases may result in non-healing ulcers, particularly on the feet and hands.
Deformities: In untreated or severe cases, leprosy can cause deformities in the hands, feet, and face.
Lagophthalmos: This condition occurs when an individual is unable to close their eyelids fully.
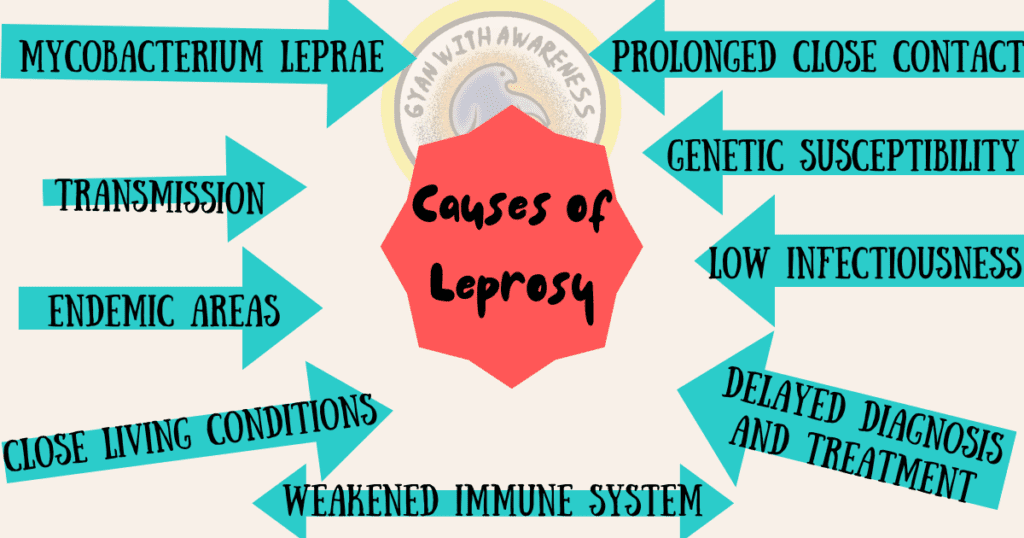
Understanding the Causes of Leprosy
Leprosy, usually referred to as Hansen’s disease, is most commonly brought on by the bacteria Mycobacterium leprae.
Mycobacterium leprae is a slow-growing bacterium, which makes it difficult to cultivate and research in the lab.
Transmission: Although the precise route of transmission is not entirely understood, it is thought to happen when an infected person coughs or sneezes through respiratory droplets.
Prolonged Close Contact: It is believed that leprosy transmission requires prolonged, recurrent, close contact with a patient who is not receiving treatment.
Low Infectiousness: Leprosy is considered to be a relatively low infectious disease, and not everyone who is exposed to the bacterium becomes infected.
Genetic Susceptibility: Some individuals may have a genetic predisposition that makes them more susceptible to contracting leprosy.
Weakened Immune System: A compromised or weakened immune system can increase the risk of developing active leprosy after exposure to the bacterium.
Close Living Conditions: Living in crowded or unsanitary conditions can facilitate the transmission of the bacterium.
Endemic Areas: Leprosy is more prevalent in certain regions of the world, particularly in tropical and subtropical climates.
Delayed Diagnosis and Treatment: Delayed diagnosis and treatment of leprosy can lead to continued transmission within communities.
Treatment for Leprosy
Here some of the tips are given below for leprosy cure:
Multi-Drug Therapy (MDT): The cornerstone of leprosy treatment, MDT involves a combination of antibiotics that target the Mycobacterium leprae bacterium.
Duration of MDT: Treatment duration depends on the type and severity of leprosy, ranging from 6 months to a year or more.
Combination Therapy: MDT typically includes drugs like dapsone, rifampicin, and clofazimine, which work together to eliminate the bacteria.
Regular Monitoring: Patients under MDT require regular follow-up appointments to assess progress and detect any potential side effects.
Management of Reactions: Some patients may experience reactions during treatment, which require additional medication to control inflammation.
Prevention of Disabilities: Physiotherapy and occupational therapy are crucial in preventing and managing disabilities associated with advanced cases.
Surgical Interventions: In cases with severe deformities or nerve damage, surgical procedures may be necessary to correct impairments.
Treatment of Complications: Additional medical attention may be needed for complications like infections or injuries to prevent further health issues.
Psychosocial Support: Addressing the social and psychological aspects of living with leprosy is integral to holistic treatment.
Health Education: Providing education on self-care, hygiene, and prevention of disabilities empowers individuals in managing their condition.
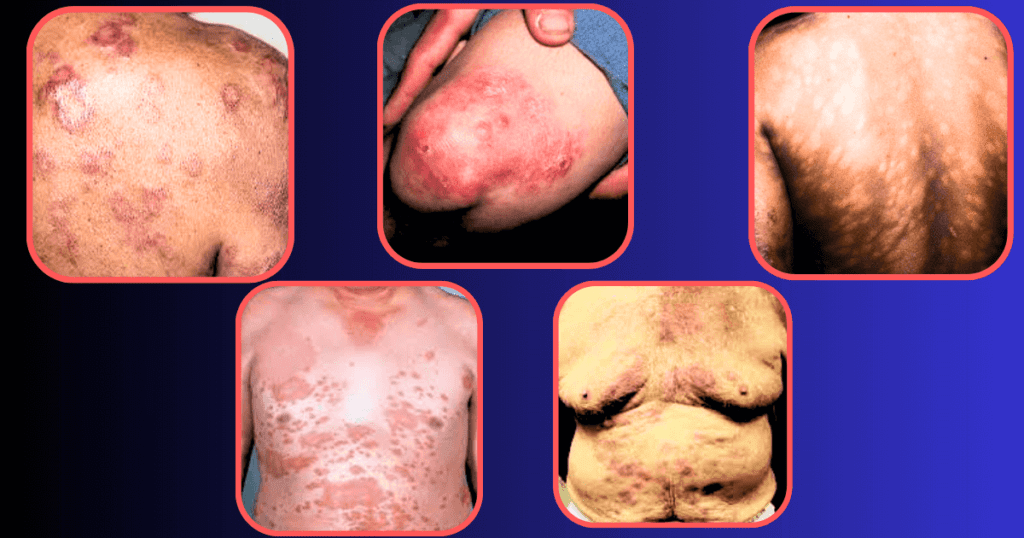
Leprosy Pictures:
Define armadillo leprosy
Armadillos play a crucial role in the transmission of this disease due to their susceptibility to bacteria and their tendency to dig and root in soil, potentially exposing humans to contaminated material. When in contact with infected armadillos, particularly through hunting or handling, humans can contract armadillo leprosy. The strain is nearly identical to the one that affects humans, making it a valuable tool for scientific research on leprosy.
The leprosy bacterial strain known as Mycobacterium leprae, also referred to as “armadillo leprosy,” only affects armadillos. It is a zoonotic illness, which means that it can spread from animals to people. The south of the United States, where armadillos are more prevalent, is where this unusual type of leprosy is most frequently found.
Although cases of armadillo leprosy in humans are relatively rare, understanding this unique strain is essential for studying leprosy transmission and developing effective prevention strategies. It underscores the interconnectedness of human and animal health and highlights the importance of wildlife management and conservation in public health efforts.
Advanced leprosy
Advanced leprosy, also known as late or severe leprosy, represents the later stages of the disease when significant damage to nerves, skin, and other tissues has occurred. This stage typically arises due to a delayed diagnosis or inadequate treatment.
In advanced leprosy, nerve involvement is extensive, leading to a range of debilitating complications. Sensory loss is profound, resulting in a lack of pain perception, which can lead to repeated injuries, infections, and subsequent tissue damage. As a result, individuals with advanced leprosy may develop severe deformities, particularly in the hands, feet, and face. Clawed fingers and toes, muscle weakness, and contractures (inflexible joint positions) are common.
The skin also undergoes significant changes. Chronic skin ulcers and wounds may form, increasing the risk of secondary bacterial infections. These infections can exacerbate tissue damage and contribute to the development of gross deformities. Additionally, advanced leprosy can lead to thickened, discolored patches on the skin, sometimes resembling leonine facies, a condition where the face takes on a lion-like appearance.
It reactions, which are sudden inflammatory responses, become more frequent in advanced stages. These reactions can cause swelling, pain, and further nerve damage. Additionally, systemic complications may arise, including kidney dysfunction, joint inflammation, and orchitis (inflammation of the testicles).
Ultimately, advanced it is a deeply debilitating condition that significantly impacts an individual’s quality of life. It highlights the critical importance of early diagnosis and prompt, comprehensive treatment to prevent progression to this severe stage and to mitigate the profound physical and psychological effects of the disease.
Do armadillos carry leprosy?
Yes, armadillos are known to carry a strain of bacteria called Mycobacterium leprae, which causes leprosy in humans. It, also known as Hansen’s disease, is a chronic infectious disease that primarily affects the skin, nerves, and mucous membranes. While it is relatively rare today, cases still occur in various parts of the world.
Armadillos are one of the few known animal species that can carry and transmit this bacterium. The link between armadillos and it was discovered through genetic analysis, which identified a close match between the strains found in infected humans and those present in armadillos. It is believed that armadillos became carriers of the bacterium from humans, as the disease is thought to have originated in ancient times.
Human infections from armadillos typically occur through direct contact with the animal’s bodily fluids, such as blood or saliva, or consumption of undercooked armadillo meat. However, it’s important to note that such cases are relatively rare, and the risk of contracting it from armadillos is generally low.
Due to the potential risk, it is advised to avoid contact with armadillos, especially if they are sick or dead. Additionally, individuals who live in regions where armadillos are known carriers of leprosy should take precautions when handling these animals or should seek professional help for their removal.
Overall, while armadillos can carry the bacteria that causes it, the risk of transmission to humans is relatively low and can be minimized with proper precautions and hygiene practices.
In conclusion, understanding the causes, recognizing the symptoms, and implementing effective treatments are crucial components in addressing and managing a range of health conditions. Each ailment has its own unique set of contributing factors, signs, and therapeutic approaches. Individuals must be informed about these aspects to ensure early detection and intervention, ultimately leading to better health outcomes.
The identification of underlying causes serves as the foundation for targeted treatment strategies. By addressing the root factors that contribute to a particular condition, healthcare providers can develop tailored approaches that aim to mitigate or even eliminate the issue. Moreover, recognizing the symptoms associated with a specific ailment empowers individuals to seek timely medical attention, preventing potential complications and facilitating a swifter path to recovery.
In all cases, collaboration between healthcare providers and patients plays a crucial role in achieving positive outcomes. The synergy between expert medical knowledge and individual participation in one’s healthcare journey is a powerful force for healing and recovery.
Also Read: Eyesight! Expert Tips for Enhancing and 8 Healthy Food
FAQ:
Is leprosy curable?
Hansen’s disease, widely known as leprosy, is treatable. It’s patients can be effectively treated and lead regular, productive lives with the help of early diagnosis and the right therapy. It is often treated with a cocktail of antibiotics called a multi-drug therapy (MDT), which frequently consists of medications like dapsone, rifampicin, and clofazimine. This mixture functions to eliminate the disease-causing germs and stop them from spreading throughout the body.
The duration of treatment varies depending on the severity of the disease and the type of leprosy diagnosed. For paucibacillary leprosy, which involves a lower bacterial load, treatment typically lasts for six months. Multibacillary leprosy, which has a higher bacterial load, requires treatment for a minimum of one year.
Early diagnosis and treatment are crucial in preventing complications and reducing the risk of disability associated with leprosy. Regular follow-up visits with healthcare providers are essential to monitor progress and adjust treatment if necessary. In addition to antibiotics, individuals with leprosy may also receive supportive care to manage any associated complications or disabilities.
It’s important to note that with prompt and proper treatment, leprosy is not only curable but the risk of transmission to others is greatly reduced. Additionally, advancements in medical science and healthcare practices have significantly improved the prognosis and quality of life for individuals affected by leprosy. Efforts to eradicate the disease and reduce the stigma associated with it continue to be important global health initiatives.
How do you get leprosy?
Leprosy, also known as Hansen’s disease, is primarily transmitted through prolonged and close contact with a person who is untreated and infectious. It is caused by the bacterium Mycobacterium leprae. Contrary to popular belief, it is not highly contagious and is much less easily transmitted than many other infectious diseases.
Though the precise means of transmission are still unclear, it is generally accepted that infected individuals cough or sneeze, which releases respiratory droplets into the air, is how the disease is spread. Direct contact with infectious nasal or oral secretions may potentially be a factor in extremely uncommon situations. It’s important to note that certain places’ armadillos, a small mammal, may harbor a form of Mycobacterium leprae that could potentially infect people. This particular form of transmission is rare, though.
Additionally,it is believed to have a prolonged incubation period, often taking several years for symptoms to manifest after initial exposure. This extended period of dormancy makes it difficult to trace the exact source of infection.
It is not very contagious, and there is very little chance that someone who comes into contact with an infected person will get it. This needs to be emphasized. Additionally, the illness is treatable with the right medical care. The key to avoiding problems and lowering the danger of transmission to others is early identification and treatment.
How is leprosy spread?
Mycobacterium leprae, which causes leprosy, is often transmitted by continuous intimate contact with an infectious, untreated person. Although the precise means of transmission are still unknown, it is thought that respiratory droplets released into the air when an infected person coughs or sneezes are the main means of transmission. Direct contact with infectious nasal or oral secretions may occasionally also aid in transmission. It is not very contagious, and there is very little chance that someone could get it simply passingly or briefly coming into contact with an afflicted person.
In rare instances, individuals can contract it from armadillos, small mammals that can carry a strain of Mycobacterium leprae. However, this form of transmission is infrequent and typically occurs in regions where contact with armadillos is more common.
Furthermore, it is characterized by a prolonged incubation period, often taking several years for symptoms to manifest after initial exposure. This extended period without visible symptoms makes it challenging to trace the exact source of infection.
Given the relatively low contagion potential and the availability of effective treatment, it is not a disease that should instigate undue fear or stigma. Early diagnosis and appropriate medical intervention are essential to prevent complications and further transmission. Through education, early detection, and accessible healthcare, leprosy can be effectively managed and treated, ultimately reducing its impact on affected individuals and communities.




2 thoughts on “Leprosy: Causes, Symptoms, and 10 Effective Treatments”